Kidney Failure: A Complete Timeline From Early Kidney Damage to Long-Term Management
Introduction
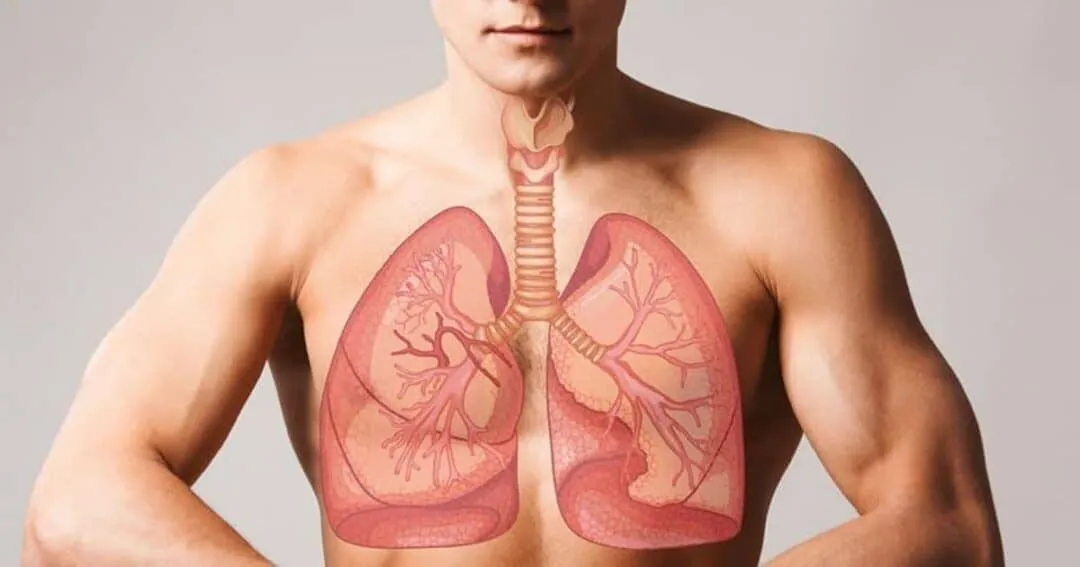
Kidney Failure is a serious medical condition that occurs when the kidneys lose their ability to filter waste and excess fluids from the blood. The kidneys play a vital role in maintaining balance within the body, regulating blood pressure, electrolytes, and red blood cell production. When Kidney Failure develops, these essential functions are disrupted, leading to widespread health consequences.
This article explores Kidney Failure as a progressive condition, beginning with early kidney stress and moving through chronic disease, advanced failure, treatment options, and long-term living strategies. Understanding this timeline helps patients recognize warning signs early and seek timely medical care.

1. The Role of the Kidneys and How Kidney Failure Begins
The kidneys are bean-shaped organs responsible for filtering toxins, balancing fluids, and maintaining electrolyte levels. Kidney Failure begins when repeated injury or chronic stress damages the delicate filtering units known as nephrons.
In the early stages, kidney damage may be mild and reversible. However, continued exposure to harmful conditions such as high blood pressure or diabetes gradually reduces kidney function, setting the stage for Kidney Failure.
Normal Kidney Function
Healthy kidneys remove waste products, regulate acid levels, and activate vitamin D. When this balance is disturbed, early signs of Kidney Failure may quietly develop without noticeable symptoms.
Early Kidney Stress
Temporary kidney stress caused by dehydration, infection, or medication misuse may recover, but repeated stress increases the risk of permanent Kidney Failure.
2. Risk Factors and Underlying Causes
Many cases of Kidney Failure are linked to chronic conditions that damage blood vessels and kidney tissue over time. Diabetes and hypertension are the two leading causes worldwide.
Lifestyle factors and genetic predisposition also play significant roles in increasing vulnerability to Kidney Failure, especially when combined with poor medical management.
Common Causes of Kidney Failure
- Diabetes mellitus
- High blood pressure
- Chronic glomerulonephritis
- Polycystic kidney disease
- Long-term use of certain medications
Additional Risk Factors
Age, obesity, smoking, and family history contribute to higher rates of Kidney Failure, especially when early symptoms go unnoticed.
3. Early-Stage Kidney Disease and Silent Progression
In the early stages, kidney disease progresses quietly. Many individuals with declining kidney function feel normal, which makes Kidney Failure difficult to detect early.
Routine blood and urine tests are often the only way to identify early kidney damage before symptoms develop.
Early Laboratory Changes
Elevated creatinine levels and protein in the urine are early markers that Kidney Failure may be developing.
Why Symptoms Are Often Absent
The kidneys can compensate for damage for years. This silent progression delays diagnosis until Kidney Failure reaches an advanced stage.
4. Mild to Moderate Symptoms of Kidney Failure
As kidney function declines, symptoms begin to appear. These early symptoms of Kidney Failure are often vague and easily mistaken for other conditions.
Fatigue, changes in urination, and swelling may signal worsening kidney function and should prompt medical evaluation.
Common Early Symptoms
- Increased or decreased urination
- Swelling in ankles or face
- Fatigue and weakness
- Difficulty concentrating
Impact on Daily Life
Although mild, these symptoms may reduce productivity and quality of life as Kidney Failure progresses.
5. Advanced Kidney Failure and Systemic Effects
When kidney function drops significantly, waste products accumulate in the blood, leading to severe symptoms. At this stage, Kidney Failure affects nearly every organ system.
Patients may experience nausea, shortness of breath, and abnormal heart rhythms due to electrolyte imbalance.
Severe Symptoms of Kidney Failure
- Persistent nausea and vomiting
- Severe swelling
- Chest pain
- Muscle cramps
Complications
Advanced Kidney Failure increases the risk of cardiovascular disease, infections, and bone disorders.
6. Diagnosis and Staging of Kidney Failure
Diagnosing Kidney Failure involves blood tests, urine analysis, imaging studies, and sometimes kidney biopsy. These tests determine the extent and cause of kidney damage.
Doctors classify Kidney Failure into stages based on glomerular filtration rate (GFR), which measures kidney efficiency.
Stages of Kidney Failure
- Stage 1: Mild damage
- Stage 2–3: Moderate decline
- Stage 4: Severe decline
- Stage 5: End-stage Kidney Failure
Importance of Accurate Staging
Correct staging helps guide treatment decisions and slows progression of Kidney Failure.
7. Treatment Options Before End-Stage Kidney Failure
Early treatment focuses on controlling underlying conditions and preventing further kidney damage. Proper management can significantly delay Kidney Failure progression.
Medications, dietary changes, and lifestyle adjustments are key components of early intervention.
Common Treatment Strategies
- Blood pressure control
- Blood sugar management
- Protein-restricted diet
- Avoiding kidney-toxic drugs
Role of Patient Education
Understanding Kidney Failure empowers patients to actively participate in their care and improve outcomes.
8. End-Stage Kidney Failure and Renal Replacement Therapy
When kidneys can no longer support life, renal replacement therapy becomes necessary. End-stage Kidney Failure requires dialysis or kidney transplantation.
This stage marks a major life transition and requires significant physical and emotional adjustment.
Dialysis Options
- Hemodialysis
- Peritoneal dialysis
Kidney Transplantation
A transplant offers the best long-term survival for eligible patients with Kidney Failure, though donor availability remains a challenge.
9. Living With Kidney Failure: Physical and Emotional Challenges
Living with Kidney Failure affects mental health, relationships, and daily routines. Depression and anxiety are common, particularly among dialysis patients.
Strong support systems and mental health care improve coping and quality of life.
Emotional Impact
- Fear and uncertainty
- Loss of independence
- Financial stress
Coping Strategies
Counseling, support groups, and lifestyle adaptation help individuals live well despite Kidney Failure.
10. Prevention, Long-Term Care, and Future Outlook
While not all cases of Kidney Failure are preventable, early detection and proper management significantly reduce risk. Preventive care focuses on controlling chronic conditions and regular screening.
Medical advances continue to improve survival and quality of life for patients with Kidney Failure.
Prevention Strategies
- Regular health checkups
- Healthy diet and exercise
- Blood pressure and glucose control
- Avoiding smoking
Advances in Kidney Care
Innovations in dialysis technology, transplantation, and regenerative medicine offer hope for the future of Kidney Failure treatment.
Conclusion
Kidney Failure is a progressive condition that unfolds over time, often without early warning signs. From initial kidney stress to advanced disease requiring dialysis or transplantation, understanding the full timeline of Kidney Failure enables early action and better outcomes.
With proper medical care, lifestyle changes, and emotional support, many individuals live meaningful lives despite Kidney Failure. Awareness, prevention, and continued research remain essential in reducing the global impact of this condition.