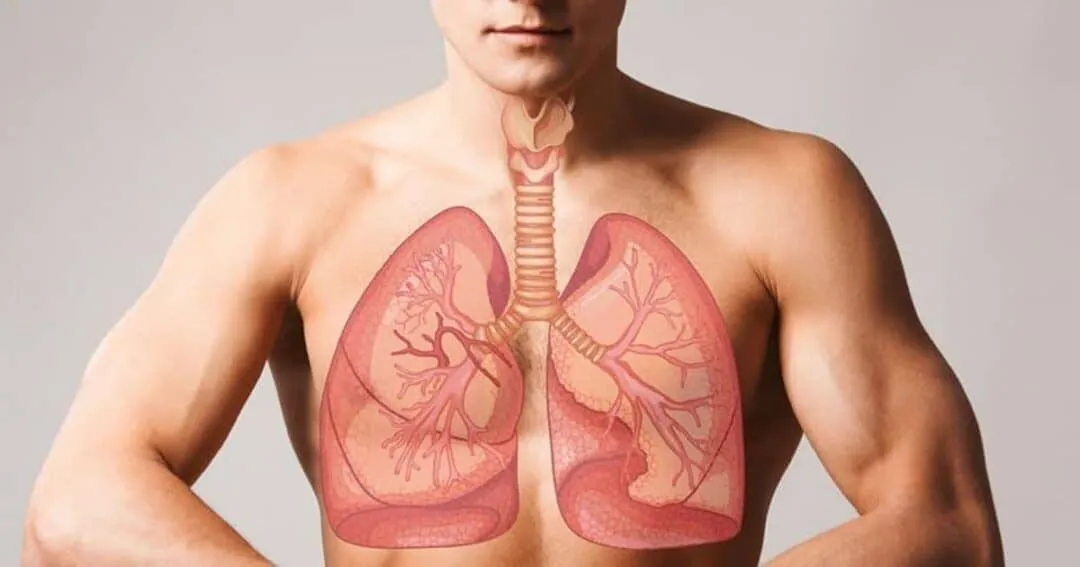
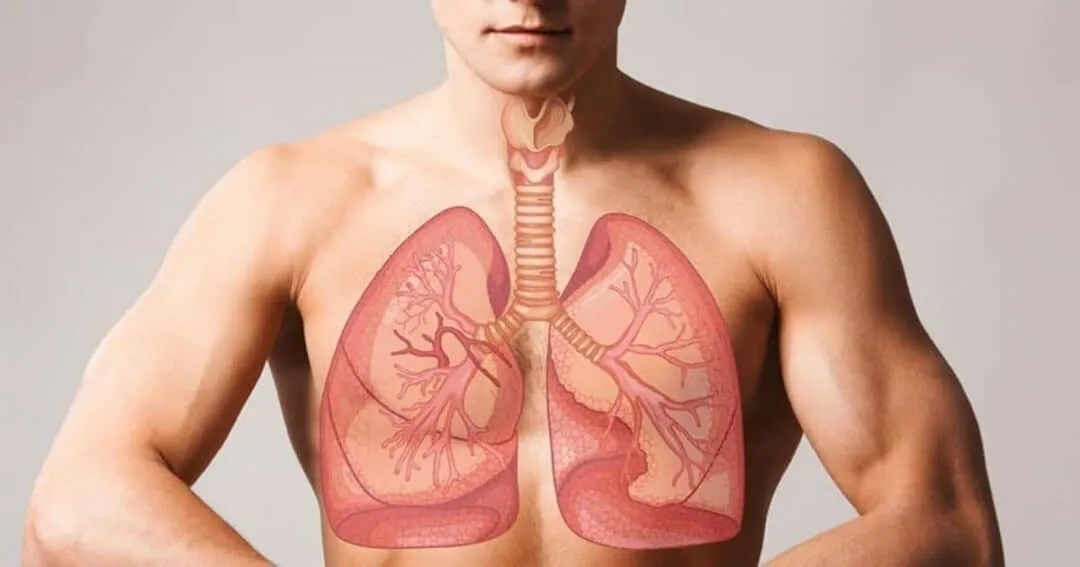
Addressing Lung Cancer Disparities in the U.S.: Closing Gaps in Access and Outcomes
Lung cancer remains a leading cause of cancer-related death in the United States, but outcomes are not the same for everyone. Differences in access to screening, early diagnosis, and advanced treatment have created measurable disparities across geographic regions, income levels, and demographic groups.
Public health experts increasingly emphasize that improving lung cancer outcomes requires addressing these systemic gaps alongside medical innovation.
Screening Availability Remains Uneven
Low-dose CT scans are one of the most effective tools for early lung cancer detection, yet access varies significantly. Rural communities and underserved urban areas often face:
- Fewer imaging centers
- Longer wait times for appointments
- Limited awareness of screening eligibility
- Transportation and cost barriers
As a result, many high-risk individuals are diagnosed at later stages, when treatment options are more limited.
Socioeconomic Factors Influence Diagnosis and Treatment
Income level, insurance coverage, and education all play a role in lung cancer care. Patients without comprehensive insurance may delay seeking medical attention or struggle to afford follow-up testing and treatment.
Healthcare providers note that financial concerns frequently lead to:
- Missed screenings
- Interrupted treatment plans
- Reduced participation in clinical trials
- Higher stress and poorer overall outcomes
Addressing affordability is increasingly seen as essential to improving survival rates.
Racial and Ethnic Disparities Continue to Be Studied
Research indicates that certain racial and ethnic groups experience higher lung cancer mortality despite similar or lower smoking rates. Contributing factors may include:
- Differences in healthcare access
- Later-stage diagnosis
- Environmental exposure
- Lower referral rates to specialists
Medical institutions are expanding research and outreach programs to better understand and address these disparities.
Community-Based Solutions Gain Momentum
To reduce inequities, healthcare organizations are implementing community-focused strategies such as:
- Mobile lung cancer screening units
- Partnerships with local clinics and nonprofits
- Multilingual education campaigns
- Patient navigation and advocacy programs
These efforts aim to meet patients where they are and remove barriers to early detection and care.
Policy and Funding Play a Growing Role
Public health advocates emphasize the importance of policy support to expand screening programs and fund lung cancer prevention initiatives. Increased funding for community health centers and public awareness campaigns is viewed as a critical step toward improving nationwide equity in lung cancer care.
Conclusion
Disparities in lung cancer care remain a significant challenge in the United States, affecting who gets screened, diagnosed, and treated in time. By expanding access, addressing socioeconomic barriers, and investing in community-based solutions, healthcare systems can move toward more equitable lung cancer outcomes. Closing these gaps is essential to reducing the overall burden of lung cancer nationwide.